
reported a lower ratio of T1 hypointensity to T2 load in PPMS (14).

In addition to finding lower lesion loads in PPMS compared to SPMS, Lycklama á Nijeholt et al. New T2 lesion load was seen to come from the enlargement of existing lesionsĪnd only 9 percent from new discrete lesions.
Ms clean mri registration#
Image registration has been used to show precisely T2 lesion load increased by a median of 7.3 percent and T1 lesion load increasedīy a median of 12.6 percent. Or more new brain lesions over a 1-year period (12). *See main text for reference note numbers.Ĭhanges in lesion number and load over time in PPMS were studied by StevensonĮt al., who found that 43.6 percent of patients with PPMS demonstrated one This article will outline the findings to date on conventional and nonconventional MR in patients with PPMS, beginning with the earliest studies designed specifically to examine patients with this form of MS. Unfortunately, limitations remain with respect to resolution and pathological specificity of the newer MRI measures. This information previously was available only by direct examination of pathological material. The resolution of structural imaging has improved, and it is now possible to use MRI to obtain information about nervous tissue, including its chemical composition and structure. The extent to which tissue can be characterized by means of MRI has increased in recent years. Magnetic resonance (MR) imaging (MRI) provides a safe and noninvasive way to study nervous tissue without the use of ionizing radiation. Potentially, understanding the nature of progression of disability in PPMS may be helpful in understanding progression in MS more generally. More speculatively, the progressive element that often ultimately develops in other clinical forms of MS may have similarities to the process that is occurring from onset in PPMS. It seems likely that the development of such treatments will be aided by insights into disease mechanisms. It is important to understand these mechanisms because PPMS is a disabling condition for which no effective disease-modifying treatment exists yet. However, how truly distinct PPMS is from relapsing-remitting MS (RRMS) remains a subject for speculation, and the issue is likely to remain unresolved until underlying pathological mechanisms are more clearly understood. Patients with PPMS differ in a number of ways from the general MS population they are likely to be older, motor symptoms are prominent at presentation, and incidence in males and females is similar (2). The progressive, nonepisodic nature and relative rarity of PPMS complicate its study, and patients routinely have been excluded from many MS clinical trials. Progressive disease from onset without relapses and remissions is seen in 10 to 15 percent of patients with multiple sclerosis (MS), and for these patients, the term primary progressive multiple sclerosis (PPMS) is now widely accepted (1).

Key words: diffusion-weighted imaging, functional magnetic resonance imaging, magnetic resonance imaging, magnetic resonance spectroscopy, magnetization transfer imaging, primary progressive multiple sclerosis, spinal cord. These techniques are sensitive to a wider range of abnormalities within tissue, and their increased pathological specificity may be helpful in clarifying the underlying pathology of the condition. Studies using newer MRI techniques, such as magnetization transfer imaging (MTI), diffusion-weighted imaging (DWI), magnetic resonance spectroscopy (MRS), and functional MRI (fMRI), have also been carried out.
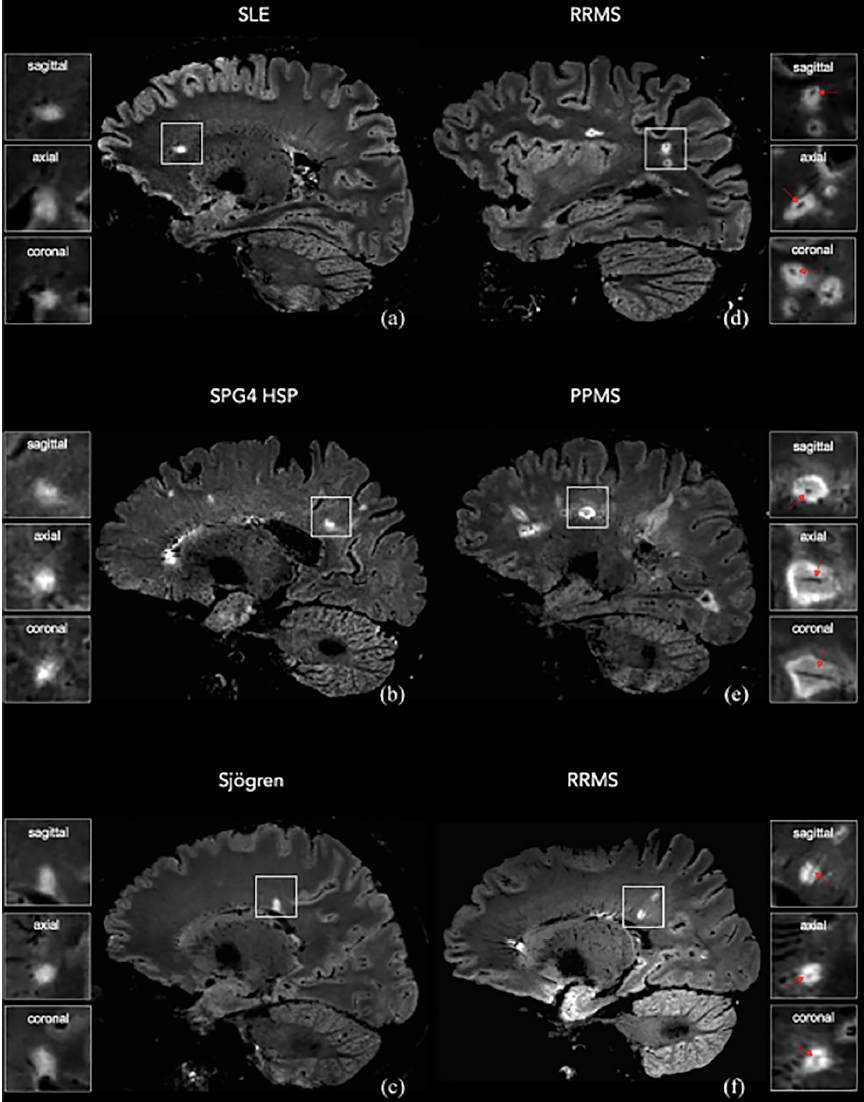
In common with relapsing MS, the relation between conventional MRI abnormalities and clinical condition is poor. The conventional magnetic resonance imaging (MRI) characteristics of PPMS include a tendency to lower lesion loads and lower rate of new lesion formation. Patients with PPMS tend to be older, often present with motor symptoms and, in contrast to relapsing MS, are as likely to be male as female. Abstract - Ten to fifteen percent of patients with multiple sclerosis (MS) have a condition that is progressive from onset without a preceding relapsing-remitting phase: this is known as primary progressive multiple sclerosis (PPMS).


 0 kommentar(er)
0 kommentar(er)
